
Infectious Disease Prevention

Infectious Disease Prevention
Student Health Services' public health efforts are dedicated to disease surveillance and prevention on campus. We provide information and resources on common communicable diseases, including COVID-19, meningitis and mpox.
On this page
Vaccine Documentation
As of June 5, 2023, UD students are strongly recommended but not required to receive COVID-19 vaccination. Student Health highly encourages students to remain up-to-date with COVID-19 vaccination, which are available through our Immunization department. Please visit the UD coronavirus website for the latest campus COVID-19 information and policies.
COVID-19 Frequently Asked Questions
Students, faculty and staff who test positive for COVID-19 should follow the University’s current COVID-19 protocols.
- Stay away from others as much as possible to prevent spread of the virus. Do not interact with anyone who is not COVID-positive or attend in-person classes, work, parties, public businesses, restaurants, bars, gyms, etc. If possible, you should not share a bedroom or a bathroom with anyone else during this time. If you must share a bedroom and/or bathroom, remain masked at all times except when eating, drinking, bathing or sleeping.
- We are here for you! If you have concerns about your symptoms or medical history, need guidance on medications to take, or have any other questions, please call SHS at 302-831-2226 between 8:30 a.m.–5 p.m. on weekdays and the Highmark Nurse Line at 888-258-3428 after hours.
If you are experiencing any potential COVID-19 symptoms (such as fever, chills, body aches, cough, shortness of breath, loss of taste or smell, sore throat, congestion, nausea, vomiting or diarrhea), you should obtain COVID-19 testing. You should not attend classes or social events until you obtain a COVID-19 test. You can utilize an at-home COVID-19 rapid antigen test kit (available at the Student Health Dispensary or Wellbeing Vending Machine in Perkins) or schedule an appointment at Student Health Services (SHS).
Medical advice is available to all students via phone through SHS at 302-831-2226 between 8:30 a.m.–5 p.m. on weekdays and the Highmark Nurse Line at 888-258-3428 after hours.
If you are experiencing serious symptoms such as shortness of breath, dizziness or chest pain, call 911 and be sure to tell the dispatcher if you suspect or know that you are COVID-19 positive.
Students, faculty and staff who are exposed to someone with COVID-19 should follow the University’s current COVID-19 protocols.
Please refer to these UD Coronavirus FAQs for COVID-19 testing information if you do not have symptoms.
Students can receive COVID-19 vaccines at Student Health Services (SHS). Please call the immunization department at 302-831-2226, Option 1 to schedule an appointment. (Other immunization services are also available at SHS.)
Invasive meningococcal disease is a rare but serious bacterial infection that occasionally infects college students and others living in relatively isolated, confined communities. Meningococcal meningitis is one presentation of this life-threatening disease. SHS wants students, faculty and staff to have up-to-date information about this disease and know how to reduce the risk of exposure.
Students: Meningitis ACWY vaccine is available at SHS. Please call 302-831-2226 to make an appointment. In an emergency, always dial 911. Please note that this vaccine is not covered by the UD Wellbeing Fee but the cost can be billed to insurance. Meningitis B vaccines are available at local pharmacies.
Employees: Please contact your practitioner or go to an emergency room.
Caution: Anyone who becomes ill with mild, flu-like symptoms should watch for more severe symptoms such as fever, headache, vomiting, rash or changes in mental status. If any of these symptoms develop, do not delay seeking medical attention.
Meningitis Frequently Asked Questions
Meningitis is an inflammation of the linings of the brain and spinal cord caused by either viruses or bacteria.
Viral meningitis is more common than bacterial meningitis and usually occurs in late spring and summer. Signs and symptoms of viral meningitis may include stiff neck, headache, nausea, vomiting and rash. Most cases of viral meningitis run a short, uneventful course. Since the causative agent is a virus, antibiotics are not effective. Persons who have had contact with an individual with viral meningitis do not require treatment.
Bacterial meningitis occurs rarely and sporadically throughout the year, although outbreaks tend to occur in late winter and early spring. Bacterial meningitis in college-aged students is most likely caused by Neisseria meningitidis (meningococcal meningitis) or Streptococcus pneumoniae. Because meningococcal meningitis can cause grave illness and rapidly progress to death, it requires early diagnosis and treatment. In contrast to viral meningitis, persons who have had intimate contact with a case require prophylactic therapy. Untreated meningococcal disease can be fatal.
Approximately 10 percent of the general population carry meningococcal bacteria in the nose and throat in a harmless state. This carrier state may last for days or months before spontaneously disappearing, and it seems to give persons who harbor the bacteria in their upper respiratory tracts some protection from developing meningococcal disease.
During meningococcal disease outbreaks, the percentage of people carrying the bacterium may approach 95 percent, yet the percentage of people who develop meningococcal disease is less than 1 percent. This low occurrence of disease following exposure suggests that a person’s own immune system, in addition to bacterial factors, plays a key role in disease development.
Meningococcal bacteria cannot usually live for more than a few minutes outside the body. As a result, they are not easily transmitted in water supplies, swimming pools or by routine contact with an infected person in a classroom, dining room, bar, restroom, etc.
Roommates, friends, spouses and children who have had intimate contact with the oral secretions of a person diagnosed with meningococcal disease are at risk for contracting the disease and should receive prophylactic medication immediately. Examples of such contact include kissing, sharing eating utensils or beverages and being exposed to droplet contamination from the nose or throat.
The incidence of meningococcal disease has declined steadily in the U.S. since a peak of reported disease in the late 1990s. Even before routine use of a meningococcal conjugate vaccine (MenACWY) in adolescents was recommended in 2005, the overall annual incidence of meningococcal disease had decreased 64 percent, from 1.1 cases per 100,000 population in 1996 to 0.4 cases per 100,000 population in 2005. In 2018, the rate of meningococcal disease in the U.S. reached a historic low of 0.1 cases per 100,000 population. Incidence of disease caused by serogroup B, a serogroup not included in the routinely recommended MenACWY vaccine, also has declined for reasons that are not known.
From 2015 to 2018, an estimated 360 cases of meningococcal disease occurred annually in the United States, representing an average annual incidence of 0.11 cases per 100,000 population. Of those with known serogroup in 2018 (N=302), 39 percent were serogroup B and 51 percent were serogroups C, Y or W- 135. The incidence of disease is highest in infants 1 year old and under, and adolescents age 16 to 20 years old.
Meningococcal disease is potentially dangerous because it is relatively rare and can be mistaken for other conditions. The possibility of having meningitis may not be considered by someone who feels ill, and early signs and symptoms may be ignored. A person may have symptoms suggestive of a minor cold or flu for a few days before experiencing a rapid progression to severe meningococcal disease.
Understanding the characteristic signs and symptoms of meningococcal disease is critical and possibly lifesaving. Common early symptoms of meningococcal meningitis include fever, severe sudden headache accompanied by mental changes (e.g. malaise, lethargy) and neck stiffness. A rash may begin as a flat, red eruption, mainly on the arms and legs. It may then evolve into a rash of small dots that do not change with pressure (petechiae). New petechiae can form rapidly, even while the patient is being examined.
Meningococcal disease can be rapidly progressive. However, with early diagnosis and treatment, the likelihood of a full recovery is increased. Early recognition, performance of a lumbar puncture (spinal tap) and prompt initiation of antimicrobial therapy are crucial. For chemoprophylaxis, the use of such prophylactic antibiotics as ciprofloxacin or rifampin is recommended for those who may have been exposed to a person diagnosed with meningococcal disease. Anyone who suspects possible exposure should consult a practitioner immediately.
The Advisory Committee on Immunization Practices (ACIP) to the Centers for Disease Control and Prevention (CDC) recommends routine vaccination for first-year college students living in residence halls. The University of Delaware requires meningitis ACWY vaccination for all incoming students living in campus residence halls and recommends meningitis B vaccine.
The vaccines for meningococcal serogroups A, C, W and Y (MenACWY; Menactra, Sanofi Pasteur; Menveo, GlaxoSmithKline [GSK]; MenQuadfi, Sanofi Pasteur) contain meningococcal conjugate in which the surface polysaccharide is chemically bonded (“conjugated”) to a protein to produce a robust immune response to the polysaccharide. Although each of the three MenACWY vaccine products uses a different protein conjugate, the products are considered interchangeable; the same vaccine product is recommended, but not required, for all doses.
Since late 2014, vaccines have become available that offer protection from meningococcal serogroup B disease (MenB; Bexsero, GSK; Trumenba, Pfizer). These vaccines are composed of proteins found on the surface of the bacteria. These vaccine products are not interchangeable; the same vaccine product is required for all doses.
MenACWY vaccines provide no protection against serogroup B disease, and meningococcal serogroup B vaccines (MenB) provide no protection against serogroup A, C, W or Y disease. For protection against all five serogroups of meningococcus, it is necessary to receive both MenACWY and MenB.
Mpox
UD is working with the CDC and Delaware Division of Public Health (DPH) to educate our campus, prepare for and respond to mpox.
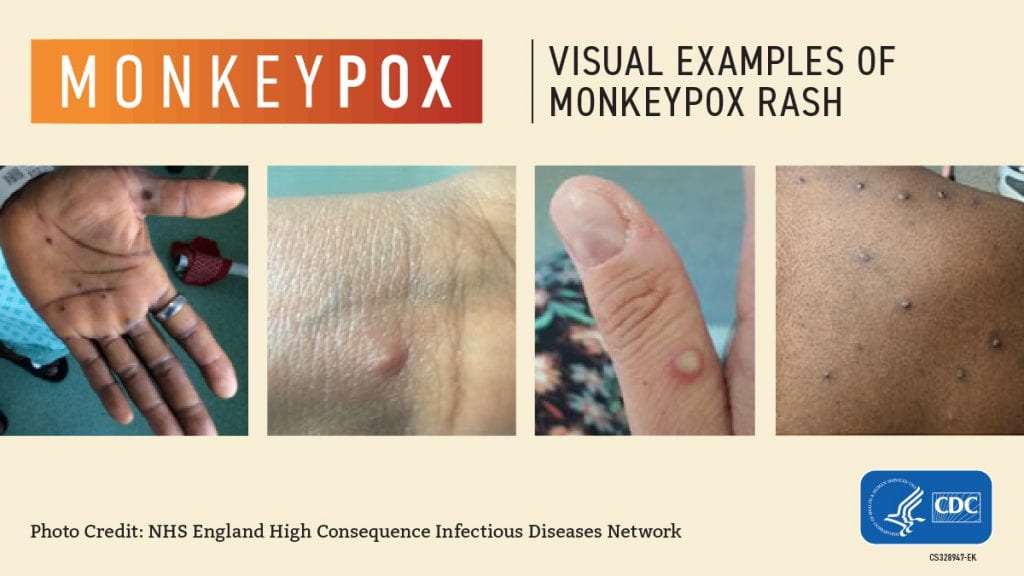
Mpox is a disease caused by a virus in the poxvirus family. It can cause fever, swollen lymph nodes and a rash. Mpox is spread through close contact, including prolonged face-to-face contact and skin-to-skin contact. It is contagious from the time symptoms begin until the rash has healed and new skin has formed. This can take two to four weeks.
Mpox Frequently Asked Questions
Mpox is a disease caused by a virus in the poxvirus family similar to smallpox. Symptoms from mpox are usually less severe than smallpox.
Infections with mpox are rarely fatal, but symptoms can be painful. Secondary skin infections can cause scarring and complications, as well.
Mpox symptoms usually start within three weeks of exposure to the virus and may include:
- Flu-like symptoms (fever, headache, muscle aches, swollen lymph nodes).
- Followed by a rash one to four days later. The rash usually begins around the mouth or face, then spreads to the hands, feet, arms, legs and trunk. Some individuals only develop a rash on or near the genitals and/or anus.
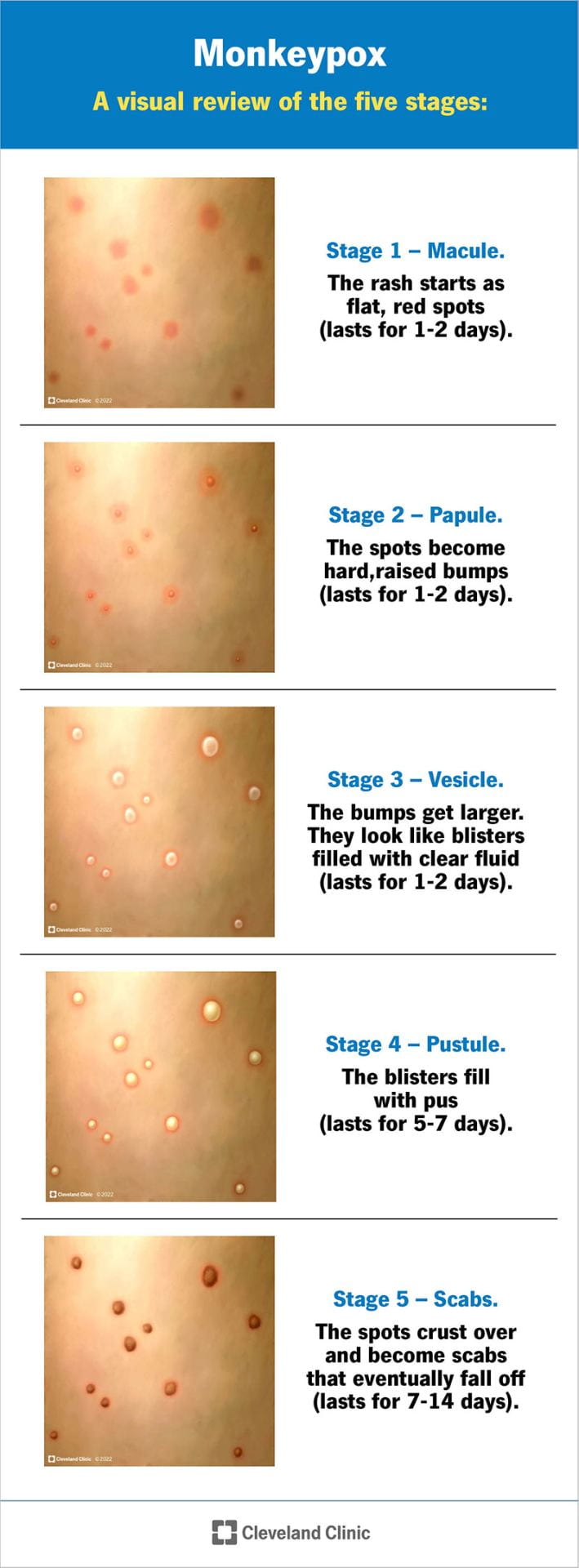
- The rash changes from small, flat red or dark spots to tiny blisters (vesicles) and then to larger, pus-filled blisters or pustules. The rash can take several weeks to heal.
- A person is contagious from the time their symptoms begin until the rash is completely healed and new skin has formed. This can take two to four weeks.
- If you have symptoms of mpox, contact SHS by calling 302-831-2226. Let them know if you have a rash or a concern about mpox. Employees should contact their healthcare provider.
- Your healthcare provider can test for mpox, if indicated.
Mpox testing is only available from a healthcare provider. There are no home tests available. Healthcare providers can only test for mpox once a rash has developed. A swab (like a Q-tip) is taken from a few lesions. Test results take three to five days. Students should reach out to SHS for possible testing. Faculty and staff should contact their healthcare provider.
Mpox spreads in different ways. The virus can spread from person-to-person through:
- Direct contact with the infectious rash or scabs.
- Respiratory droplets during prolonged face-to-face contact (less than three hours) or during intimate physical contact, such as kissing, cuddling or sex.
- Touching cloth items such as clothing, sheets or towels that have been used by someone with mpox.
- Touching contaminated items such as door knobs, electronics and environmental surfaces that have been used by someone with mpox.
- Sharing drinks, utensils and toothbrushes.
It is currently unknown if mpox is sexually transmitted. Unlike COVID-19, mpox does not spread by persons without symptoms or by casual contact.
- It is important to note that anyone can get mpox if they have very close contact with someone who is infected.
- Mpox spreads in close-knit social groups. A person’s individual risk is dependent on the amount of interactions with at-risk social circles and spaces.
- Your level of risk increases if you have multiple sexual partners or are engaging in social activities where there is skin-to-skin contact.
- Currently, cases are predominantly among men who have sex with men. This may include men who identify as gay, bisexual, heterosexual or any man who engages in sexual activity with other men.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
- Avoid close contact with and handling linens of people with mpox.
- Avoid touching contaminated objects that have been used by people with mpox.
- Avoid enclosed spaces where there is intimate or sexual contact.
- Avoid parties or clubs where there is direct, personal, skin-to-skin contact.
- Have open discussions with any sexual partners about symptoms of mpox and do not engage with anyone with potential symptoms.
- Get vaccinated if you are eligible.
There are increasing cases of mpox in the United States. At this time, the risk of mpox in Delaware is believed to be low. However, anyone in close contact with a person with mpox can get it and should take steps to protect themselves.
Unfortunately, condoms do not prevent mpox. Condoms are still important, as they help prevent sexually transmitted infections like HIV, gonorrhea and chlamydia.
Your level of exposure to someone with mpox depends on the timeline of their symptom onset, the duration you spent together, the proximity and the activity.
If you had a known intermediate- or high-risk exposure to someone with mpox:
- Monitor for symptoms for 21 days.
- Call SHS at 302-831-2226 if symptoms or a rash develop. Employees should contact their healthcare provider.
- Get vaccinated (see vaccine resources at the end of this page).
- Clean any shared spaces.
As of October 4, 2022, vaccines are available to:
- People with known or suspected exposure to mpox
- Individuals who are HIV+
- Individuals taking PrEP for HIV prevention
- All gay, bisexual, transgender or nonbinary persons who have sex with men
- Females having sex with gay, bisexual, transgender or nonbinary males
- Transgender women or nonbinary persons assigned male at birth who have sex with men
- Sex workers of any gender and sexual orientation
- Immunocompromised persons (including those with cancer, solid organ or stem cell transplants, those taking immunosuppressive therapy and individuals with autoimmune disease)
- Those treated for a sexually transmitted infection (STI) in the last six months
- People experiencing homelessness
- People in prison
- Healthcare workers who are providing direct patient care to confirmed or suspected mpox cases in areas such as emergency departments, urgent cares, federally qualified health centers, DPH clinics, STI/HIV or sexual health clinics and those at occupational risk, such as laboratory staff that handle mpox specimens
For vaccine information and appointments, please contact DPH at 866-408-1899 or DPHCall@delaware.gov. See the bottom of this webpage for additional vaccine resources in Delaware.
Follow the instructions from the CDC and your medical provider. The University of Delaware expects that individuals who test positive for mpox will comply with Delaware Division of Public Health communications and recommendations, including isolation and contact tracing. Individuals will need to isolate until they are no longer contagious and all scabs/lesions have resolved and new skin has grown (which can take two to four weeks). Students must return home for their isolation period. If returning home is not possible, students should reach out to their RA. Detailed isolation and cleaning instructions for mpox can be found on the CDC website.
Employees should reach out to their HR liaison for questions about leave or returning to work.
Most people with mpox recover fully within two to four weeks without the need for medical treatment. Antivirals, such as tecovirimat (TPOXX), may be recommended for people who are more likely to get severely ill, like patients with weakened immune systems. TPOXX is currently only available through the Strategic National Stockpile.
Please refer to the CDC Case Trends for the most up-to-date information. State of Delaware case counts are available through DPH.
State and Federal
- DHSS Mpox Press Release
- CDC Mpox
- CDC Reducing Mpox Transmission in Congregate Living Settings
- CDC Disinfection of the Home and Non-Healthcare Settings
- Division of Public Health: Mpox
Vaccination Resources
DPH Clinics
Call the DPH Hotline at 866-408-1899 to schedule an appointment with a public health clinic.
More Resources for Students
DPH Mpox and Vaccine Information Center
1-866-408-1899
DPHCall@delaware.gov
Respiratory Viruses
Explore the differences in symptoms, treatments and UD protocols for various respiratory viruses.
| COVID-19 | Influenza | Other Respiratory Viruses | |
|---|---|---|---|
| Cause | SARS-CoV-2 virus | Influenza A or Influenza B virus | Respiratory Syncytial Virus (RSV), Parainfluenza, Adenovirus, Rhinovirus, Enterovirus |
| Symptoms (* most common) |
|
|
|
| Treatment (Over-the-counter medications available at the SHS Dispensary) |
|
|
|
| Antivirals | Prescription antiviral medications like Paxlovid for patients at risk for complications. | Prescription antiviral medications like Oseltamivir for patients at risk of complications. | No antiviral medications available for these conditions. |
| Antibiotics | Antibiotic medications are not effective for viral illnesses. | Antibiotic medications are not effective for viral illnesses. | Antibiotic medications are not effective for viral illnesses. |
| Typical Duration | 5–10 days | 5–7 days | 7–10 days |
| Testing | Home rapid antigen test kits available at the Student Health Dispensary or Wellbeing Vending Machine in Perkins. Rapid antigen testing available with an appointment at SHS. |
Rapid antigen testing available with an appointment at SHS. |
Not routinely available. |
| Vaccination | Recommended to remain up-to-date with COVID-19 vaccination. COVID-19 vaccines are available at SHS (call 302-831-2226, Option 1, to schedule) or local retail pharmacies. |
Recommended every fall for everyone age six months and older. Available at SHS (call 302-831-2226, Option 1, to schedule). |
Not routinely available. |
| At Risk for Complications |
|
|
|
| What Should I Do at Home? |
|
|
|
| When to Seek Medical Care (SHS or Urgent Care) |
|
|
|
