Uncovering molecular pathways
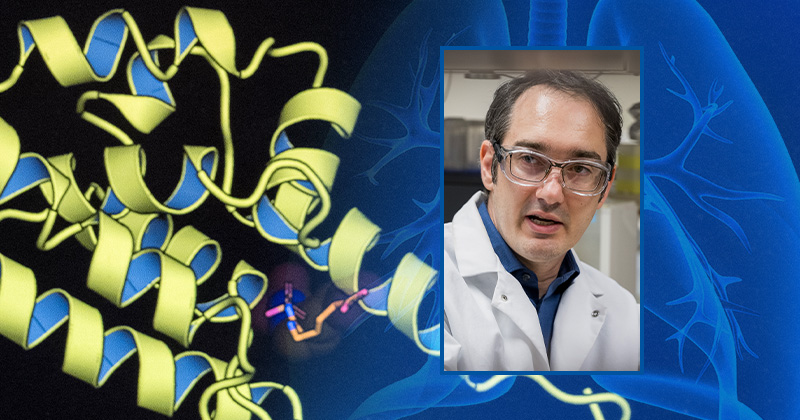
Photo by Kathy F. Atkinson | Photo illustration by Jaynell Keely November 07, 2024
UD research could lead to new treatments for tuberculosis
You might think of tuberculosis (TB) as a disease of the past, similar to polio or smallpox. In fact, it is the world’s most infectious killer, according to the World Health Organization, causing an estimated 1.5 million deaths annually. Up to one-fifth of the global population, including 13 million Americans, have TB, although most cases are in a dormant, or inactive, form.
TB is treatable with antibiotics, but up to 5% of infections are now resistant to drugs. New research by University of Delaware biology professor Karl Schmitz may provide a pathway to the development of new treatments.
Schmitz, an assistant professor in the Departments of Biological Sciences and Chemistry and Biochemistry, recently received a $1.88 million, five-year R01 grant from the National Institutes of Health (NIH) and the National Institute of Allergy and Infectious Diseases (NIAID) to map the basic biology of the bacterium that causes the disease, focusing on the specific role of unusual chemical modifications of its cellular proteins, called phosphoarginine.
These modifications can help the bacteria survive environmental stresses. Schmitz and his team are working to understand the connection between the modifications and certain enzymes they interact with that are promising targets for new antibacterial drugs.
The science
Schmitz’s research lab studies protease enzymes in TB-causing bacteria. These enzymes play critical roles in bacterial physiology. Previous work by his lab found that these proteases interact with proteins carrying phosphoarginine modifications, but the significance of the interaction was unclear.
Recent work by doctoral students Henry Anderson and Pratistha Kandel suggests that phosphoarginine changes the activity of these enzymes as part of a cell-wide pathway that helps the bacteria survive environmental stresses, which may be important for infection.

"Understanding how phosphoarginine influences protease function will help us develop drugs that interfere with protease activity, and ultimately help us treat drug-resistant TB infections,” Schmitz said.
Schmitz’s research is now exploring what triggers the creation of these protein modifications.
“We don't know which stresses specifically activate the pathway,” Schmitz said. “We know that these modifications exist, and we have pretty good evidence that their levels are modulated in concert with stress, but the upstream part that connects stress to the actual modification has not yet been mapped.”
The team is also examining the “downstream” aspects of the pathway, such as how changing phosphoarginine levels alters the cell’s behavior, and how this helps the bacteria survive stress.
“It's like a puzzle, and the pieces that we have right now are in the very middle of it,” Schmitz said. “All of the surrounding stuff is uncharted territory.”
Public health impacts
The work could have enormous implications for public health around the globe, especially in countries where TB is a serious issue. Though the disease is controlled in wealthier nations, nearly half of the people with TB live in only eight countries: Bangladesh, China, India, Indonesia, Nigeria, Pakistan, Philippines and South Africa.
“There might not be a lot of cases in the U.S., but where I'm from, for example — Nepal — there are still a lot of tuberculosis cases. People are really struggling,” Kandel said.
“It’s particularly rewarding to study a disease that disproportionately impacts regions with limited research resources,” Schmitz said.
Despite the potential impact, the team is staying focused on the science of what Schmitz calls “new biology” as this area has been previously unexplored.
“It’s hard to think about the magnitude of tuberculosis every day,” Anderson said. “But to be able to work on novel pathways that could actually make a difference is really cool.”
Contact Us
Have a UDaily story idea?
Contact us at ocm@udel.edu
Members of the press
Contact us at mediarelations@udel.edu or visit the Media Relations website